-
Adult Bone Marrow Transplantation
-
Adult Intensive Care Unit
-
Advanced Gynecology Institute
-
Anesthesiology
-
Bariatric and Metabolic Surgery
-
Breast Clinic
-
Burjeel Kidney Transplant Center
-
Cardiac Sciences
-
Clinical Nutrition and Dietetics
-
Co-Lab
-
Cosmetology and Dermatology
-
Dental
-
Emergency Medicine
-
Endocrinology
-
ENT Head & Neck Institute
-
Family Medicine
-
Gastroenterology
-
Gastrointestinal Surgery
-
General Medicine
-
General Surgery
-
HBOT (Hyperbaric Oxygen Therapy)
-
Hematology
-
Hepatopancreatobiliary Surgery and Transplantation
-
Infectious Diseases
-
Internal Medicine
-
Kypros Nicolaides Fetal Medicine & Therapy Center
-
Medical Oncology
-
Neonatology
-
Nephrology
-
Neurology
-
Neurosurgery
-
Nuclear Medicine
-
Obstetrics and Gynecology
-
Ophthalmology
-
Oral and Maxillofacial Surgery
-
Orthopedics and Sports Medicine
-
Paley Middle East Clinic
-
Palliative and Supportive Care
-
Pediatric Bone Marrow Transplantation
-
Pediatric Cardiology
-
Pediatric Endocrinology
-
Pediatric Gastroenterology
-
Pediatric Hematology
-
Pediatric Intensive Care Unit
-
Pediatric Neuroscience
-
Pediatric Oncology
-
Pediatric Pulmonology
-
Pediatric Surgery
-
Pediatrics
-
Physiotherapy, Pain Medicine & Advanced Rehabilitation
-
Plastic, Reconstructive and Cosmetic Surgery
-
Psychiatry
-
Psychology
-
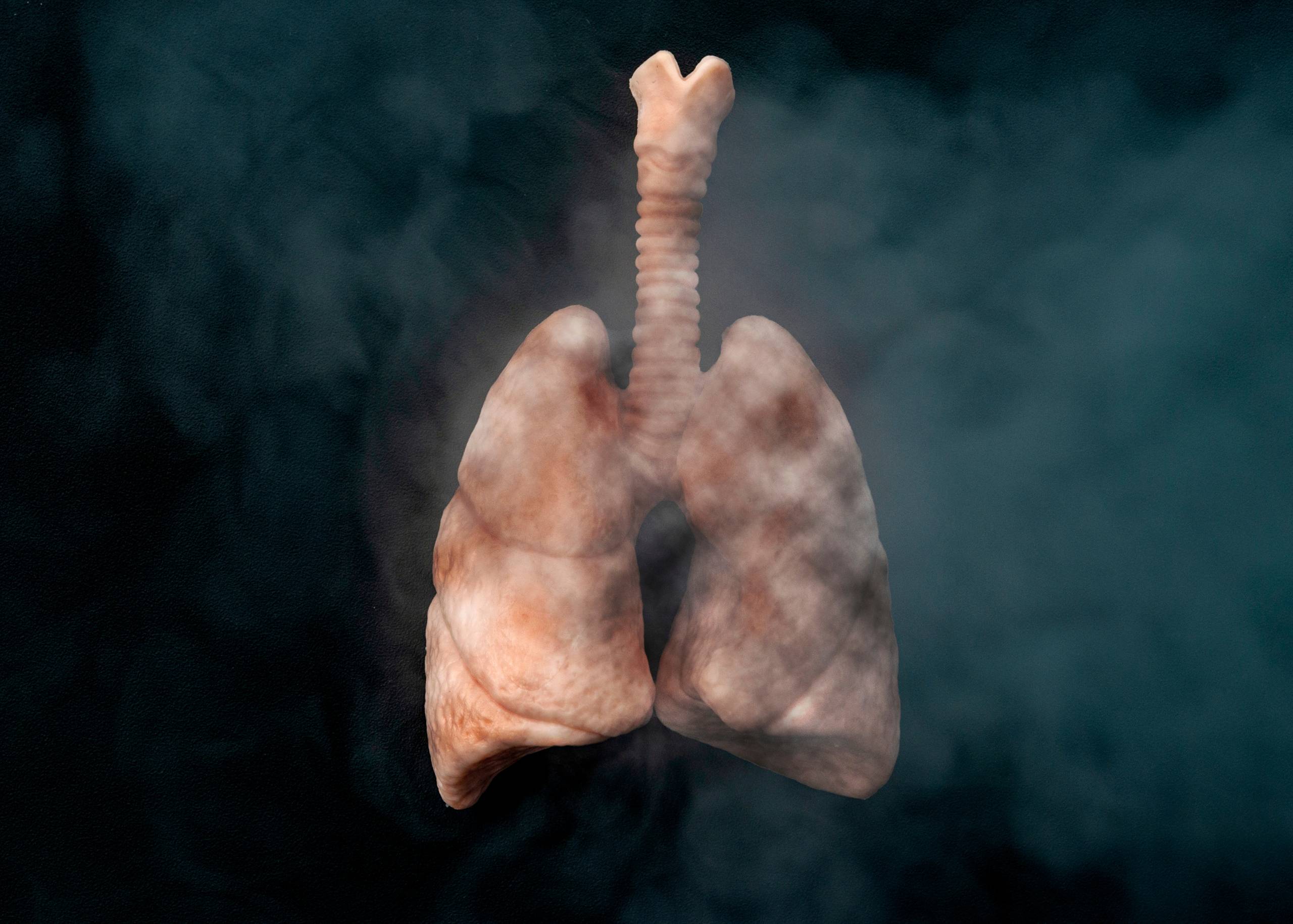
Pulmonology
-
Radiation Oncology
-
Radiology
-
Rheumatology
-
Surgical Oncology
-
Thoracic Surgery
-
Urology
-
Vascular Surgery
-
Weight Management Clinic
The Medical Oncology department at Burjeel Medical City, Abu Dhabi, is a cornerstone of our comprehensive cancer care program. Our department is dedicated to the diagnosis, treatment, and management of all cancer-related conditions, offering patients hope and healing through a combination of advanced therapies.
Our oncologists are at the forefront of cancer treatment, utilizing surgery, chemotherapy, radiation therapy, and targeted therapies to fight cancer on all fronts. Our approach is personalized, recognizing that each patient’s journey is unique, and requires a tailored treatment plan.
We are equipped with cutting-edge diagnostic tools such as CT, MRI, and PET scans, ensuring that our cancer diagnosis is precise and that treatments are effective. Our Key Differentiators highlight our commitment to democratizing innovation in cancer care and emphasizing the importance of clinical trials in advancing treatment.
List of Services
- Surgery for cancer treatment
- Chemotherapy
- Radiation therapy
- Targeted therapy
Conditions Treated
- All conditions related to cancer
Technology/Equipment
- CT scans
- MRI scans
- PET scans
Key Differentiators
- ESMO Accredited Medical Oncology & Palliative Care Center
- Democratizing innovation in oncology care
- Emphasis on clinical trials and advanced therapies
- Comprehensive cancer treatment modalities